World's First AI Powered Digital Human Cardiac Coach
〰️
World's First AI Powered Digital Human Cardiac Coach 〰️
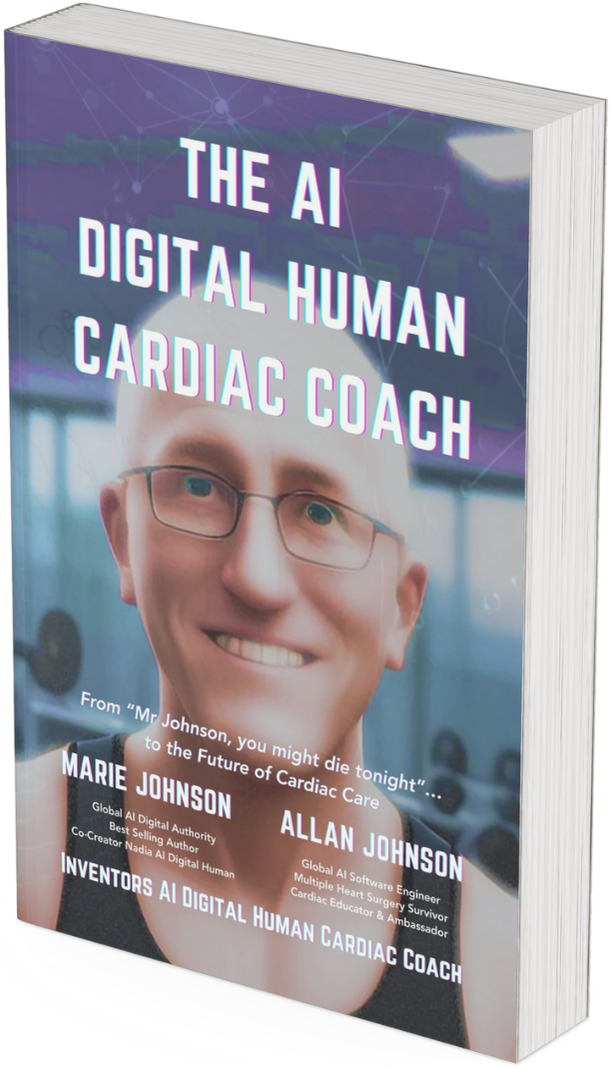
Digital Human Li from Trulience Introducing the Book
‘The AI Digital Human Cardiac Coach’
‘A life-altering health event rapidly spirals into a harrowing journey through the labyrinth of jargon-laden information.
Both revealing and inspiring, the authors transform their personal struggles into groundbreaking innovation: the world-first ‘digital human' cardiac coach.
A fascinating tale of personal resilience and cutting-edge technology, this story offers a hopeful glimpse into the future of healthcare.’
Dr Chris Hillier, CEO Angry Health
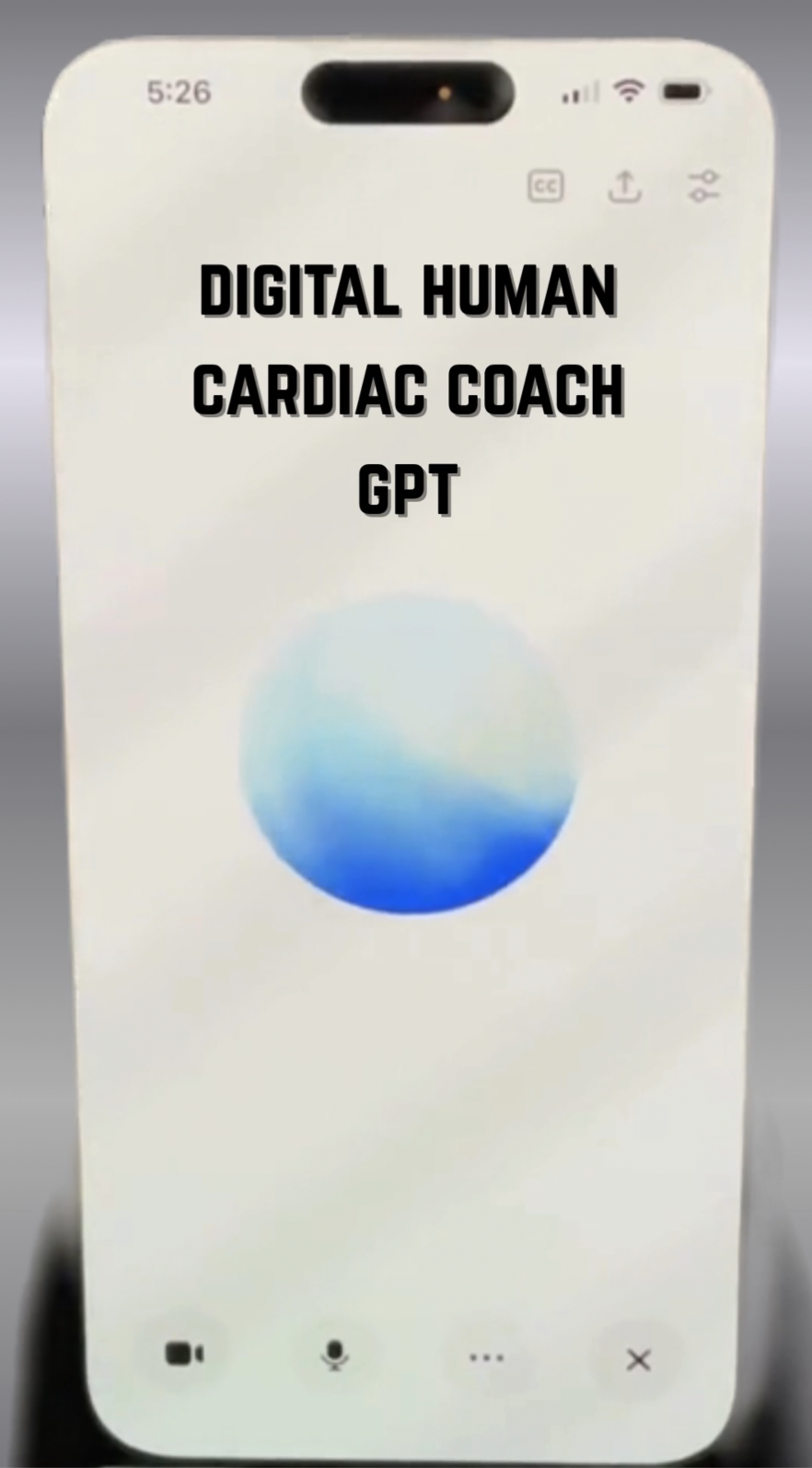
The Digital Human Cardiac Coach Becomes a
Custom GPT Agent